Researchers at Washington University School of Medicine in St. Louis, in collaboration with Northwestern University, have developed an innovative, non-invasive treatment strategy for glioblastoma. This is one of the most aggressive and difficult-to-treat brain tumours.
The new approach uses nanomedication that can be delivered directly to the brain via simple nasal drops. This technology activates powerful immune pathways that are normally difficult to reach, offering a promising alternative to current, often very stressful treatment methods.
Glioblastoma develops from astrocytes, a type of brain cell, and affects around 1,000 to 1,200 people in the United Kingdom every year. The disease progresses extremely rapidly and is almost always fatal. A major challenge in treatment is that drugs have difficulty reaching the brain due to the blood-brain barrier. Moreover, glioblastoma is known as a “cold tumour”: a tumour that hardly elicits a natural immune response, making conventional immunotherapies largely ineffective. The findings of the new research were published in PNAS earlier this month.
Activating the immune system
The research team wanted to break through this reality by reactivating the immune system. They focused on the STING (Stimulator of Interferon Genes) signalling pathway, a key mechanism that activates the immune system when cells detect foreign DNA. STING activators already exist, but they break down quickly in the body and must be injected directly into the tumour. This is an invasive procedure that must be repeated to achieve sufficient effect.
To solve this problem, the researchers collaborated with nanotechnology expert Chad Mirkin of Northwestern University, inventor of spherical nucleic acids (SNAs). These are unique nanostructures in which DNA or RNA fragments are arranged closely around a gold core, resulting in a much higher therapeutic potential than traditional delivery methods.
DNA fragments
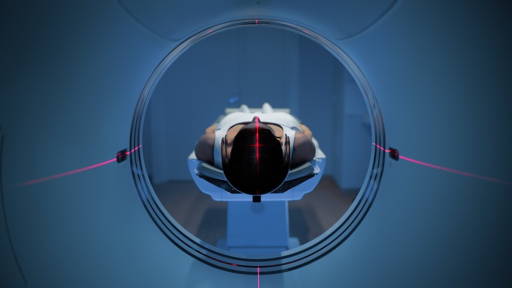
In this study, SNAs were developed that contain specially designed DNA fragments to activate the STING pathway in selected immune cells. The researchers then opted for intranasal administration, a route that is less stressful for patients and allows drugs to travel directly to the brain via nerve pathways in the nose. Until now, activating the immune system with nanoscale therapy via the nose had not been demonstrated before.
The results are promising. In mice with glioblastoma, the nanomedication selectively reached the brain, primarily activated immune cells in and around the tumour, and did not cause harmful spread to other organs. The STING pathway was strongly activated, enabling the immune system to attack tumour cells much more effectively.
The impact was even greater when the treatment was combined with agents that activate T cells. In just one or two doses, tumours were completely eliminated and long-lasting immunity was also achieved, an important advantage in a disease that almost always recurs.
Impressive results
Although the results are impressive, research leader Alexander Stegh emphasises that STING activation alone is not enough to definitively combat glioblastomas. Tumours have multiple ways of suppressing immune responses. The team is therefore working on nanostructures that can activate multiple immune signals simultaneously, making treatments more powerful and targeted.
This intranasal nanomedicine technology could lead to a new generation of brain tumour therapies: safer, less invasive and much more effective. It also opens up the prospect of treating other immunotherapy-resistant cancers.
Nanotechnology and brain tumours
In 2023, a Canadian research team developed a promising nanotechnological approach for the treatment of glioblastoma. The researchers used iron oxide-filled carbon nanotubes which, thanks to an antibody coating, bind specifically to glioblastoma cells. Once the cancer cells absorb the tubes, a magnetic field is activated, causing the nanotubes to rotate. This causes severe damage to the internal structures of the tumour cells, especially the mitochondria, and acts like thousands of mini scalpels destroying the cells from within.
In mice, this method led to a clear reduction in tumour size and an extension of life expectancy from an average of 22 to 27 days. The researchers see the technique as a Trojan Horse strategy and want to further refine the process before human trials become possible.
Earlier this year Harvard Medical School researchers developed PICTURE, an AI tool that distinguishes between glioblastoma and primary CNS lymphoma during surgery, two brain cancers that require very different treatments. Misdiagnosis can lead to unnecessary surgery or delayed therapy, making rapid, accurate identification essential.
PICTURE analyzes tumor tissue in near real time and achieved over 98% accuracy across international test sites, outperforming pathologists and previous AI models. Its key advantage is an uncertainty detector that warns clinicians when confidence is low, helping avoid risky decisions. Unlike traditional frozen-section analysis, which is fast but error-prone, PICTURE detects subtle tumor features invisible to the human eye and reduces diagnostic revisions.