Researchers at the Mayo Clinic have developed a new 3D surface scanning technique that allows neurosurgeons to navigate even more accurately during complex procedures deep within the brain. The system links the patient's head, facial features and surgical frame to brain images in a single digital environment. This achieves a precision of less than one millimetre, a margin that can make all the difference in delicate neurosurgery.
A feasibility study, published in the Journal of Neurosurgery, shows that this 3D scanning method is more accurate than the CT scans currently in standard use and does not expose patients to radiation. The technique can make procedures such as deep brain stimulation (DBS), drainages and biopsies safer, more efficient and more comfortable. Because the system is compatible with most navigation platforms, it can also enable high-precision surgery in operating theatres without a CT scanner.
How the 3D technology works
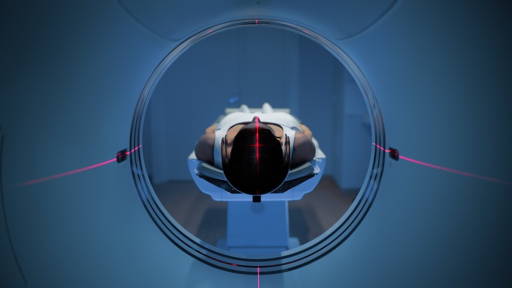
Using cameras and structured light scanning, the system creates highly detailed 3D models of the patient's face and the fixation bracket that stabilises the head. These models are combined into an accurate spatial ‘map system’ that shows the patient's position in the operating theatre. This map is then linked to preoperative MRI or CT images, allowing surgeons to see exactly where they are in the brain.
In the study, the computer-controlled analysis achieved an average alignment accuracy of 0.14 millimetres, compared to approximately 0.20 millimetres with CT scans. The difference is small, about the width of a pencil point, but in neurosurgery, it can determine whether an instrument reaches exactly the right structure.
Multidisciplinary innovation
The project brings engineering and clinical practice together. ‘When engineers and neurosurgeons look at the same problem, we see different details, and that's where breakthroughs happen. We are building the next generation of surgical tools with engineering precision down to the sub-millimetre level,’ says computational biologist and AI researcher Dr Jaeyun Sung, who led the technical development.
Neurosurgeon Dr. Kendall Lee, responsible for clinical integration, sees immediate added value: ‘Important steps take place before the first incision. This 3D method is safe, fast and cost-effective, and helps us work more accurately and thus improve the quality of care.’ Lead author Dr Basel Sharaf emphasises that the technology is just the beginning: ‘In the future, 3D scanning could become as easy as using a smartphone. With advanced AI, the system can move in real time and even predict minute shifts in brain tissue.’
The team is now working on further automation and integration of AI to speed up and simplify the workflow. In addition, new hardware designs are being tested and a larger clinical study is being launched to further validate the effectiveness of the technique in practice. This development marks an important step towards more precise, safer and widely accessible neurosurgery, where technology and clinical expertise come together for better patient outcomes.
Ultrasound innovation
This summer, researchers from Erasmus MC's BrainEcho Lab presented an innovative ultrasound device that can measure brain activity in extreme detail and in real time, even while a patient is walking. The system, which captures 10,000 images per second, was successfully tested for the first time on a moving patient thanks to a special helmet with an ultrasound holder. This uses PEEK, a plastic that sometimes replaces skull bone and allows ultrasound to pass through easily.
This technological breakthrough enables brain research during natural movements and rehabilitation. In addition, the technique can provide surgeons with insight into blood flow and vital brain areas during brain surgery, although the method has not yet been approved for intraoperative decision-making. The method also offers potential after surgery: PEEK closures enable long-term and accessible monitoring, for example as an alternative to delayed MRI scans. This can provide patients with faster clarity about recovery and the possible return of a tumour.